Tuberculosis (TB) treatment can take anywhere from 6-9 months, and even up to two years if it's drug-resistant. This long treatment period puts heavy economic pressure on many patients and their families. TB creates a double burden - it not only affects health but also brings economic stress, with patients and their families facing reduced income and the risk of falling into poverty due to illness. The most dangerous thing about detecting and treating tuberculosis is that many patients hide their illness because they fear the high costs of long-term TB treatment.
70% of TB patients have limited economic means
Vietnam is among the top 30 countries with the highest burden of multidrug-resistant TB, with over 169,000 people infected and 13,000 deaths each year (WHO report, 2022). Notably, about 70% of TB patients come from poor and near-poor households, facing significant economic and living challenges (Ministry of Health, 2023).
Poor hygiene is a major reason why TB bacteria spread easily. Cramped, humid areas, crowded populations, and poor ventilation systems create favorable environments for bacteria to grow. For homeless people or those without stable housing, factors like malnutrition and weakened resistance increase the risk of contracting and developing TB.
For those living in mountainous, remote, and isolated areas, accessing health services is difficult due to lack of transportation, distance to medical facilities, and language and cultural barriers for ethnic minorities. Lack of information about the disease and support policies further widens the gap in treatment participation, especially when the sick person is the family's breadwinner, creating concerns about stopping work during treatment or the cost of treatment being unaffordable.
All these factors not only increase disease rates but also create a cycle of poverty and illness, pushing families into even more difficult situations.
The economic burden of TB on poor patients
TB is not only a health burden but also a long-term economic pressure for the patient's family, especially poor households. Statistics show that 63% of families of TB patients face "catastrophic medical costs" - defined as costs for all health care activities exceeding 20% of annual income, causing many families to fall into poverty.
The economic impact of TB is evident in alarming figures: 26% of patients have to stop working for more than 6 months due to health problems, 5% are forced to sell assets to cover hospital fees, and 17% have to borrow money to continue treatment, while their average income decreases by 25%.
One of the key goals in the WHO's Sustainable Development Goals (SDGs) by 2030 is to achieve Universal Health Coverage (UHC) - ensuring everyone has access to safe, quality health care services whenever they need it, without financial burden. However, for TB, there are still gaps in achieving UHC as medical costs create a huge burden for patients.
Ms. Nguyen Thi Kim Dung, Program Manager of the Centre for Supporting Community Development Initiatives (SCDI), emphasized: "Although the cost of TB treatment is covered by Health Insurance, more support is still needed to minimize the financial burden on patients and families. When economic pressure is reduced, the patient's treatment compliance rate will increase, thereby preventing the risk of drug-resistant TB and protecting public health more effectively.”
Practical support policies are not only medical solutions but also contribute to ensuring stability for families affected by TB, creating a foundation for comprehensive recovery in both health and economic life.
Support policies: motivation to help TB patients overcome difficulties
The Health Insurance Policy that covers TB treatment costs is considered a humane decision, helping to reduce financial burden and ensure the treatment process is not interrupted. However, in addition to medical support, implementing social support programs is also crucial, helping TB patients and their families overcome daily life challenges.

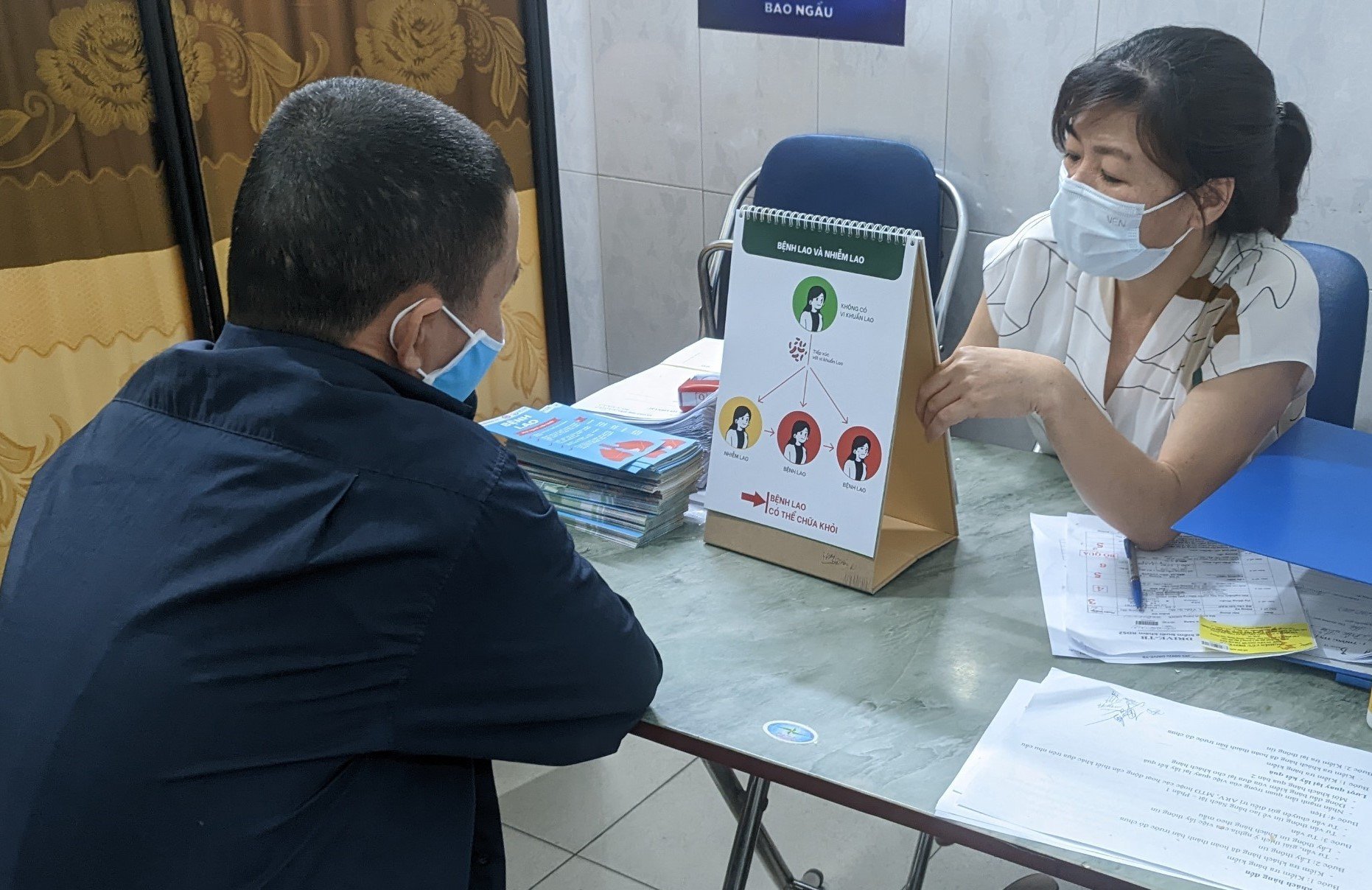
Photo: Nutritional support for TB patients during treatment.
Priority support should be given to patients with particularly difficult circumstances, those with identification document issues, lacking health insurance cards, living in remote areas, or facing language and cultural barriers. These supports not only create conditions for patients to access treatment but also encourage them to comply with the treatment regimen, reducing the risk of disease spread and recurrence.
Ms. Kim Dung emphasized: "To ensure that patients are cured and treatment is not interrupted, we need more specific support programs, contributing to building a healthier and fairer society."
Integrating social security policies into TB prevention and control programs is considered a long-term solution, helping patients reduce their economic burden and stabilize their lives, leading to the goal of TB elimination in the community.


.jpg)

.jpg)

.jpg)
%20-%20Ngh%E1%BB%87%20An.jpg)
.jpg)
.jpg)
